Some Walks in Life Are More Special Than Others
When a baby is born, we look forward to all the milestones they…
The Journey from Prototype to Production: Part 2
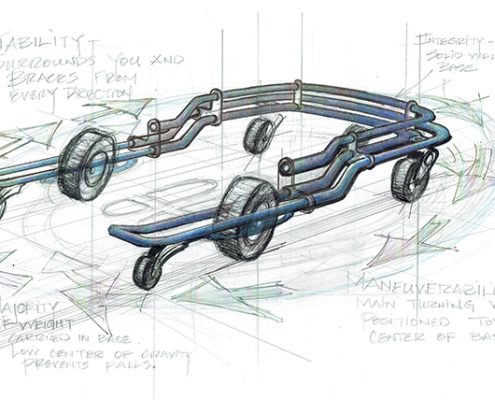
After designing the first U-Step, I decided to continue on the…

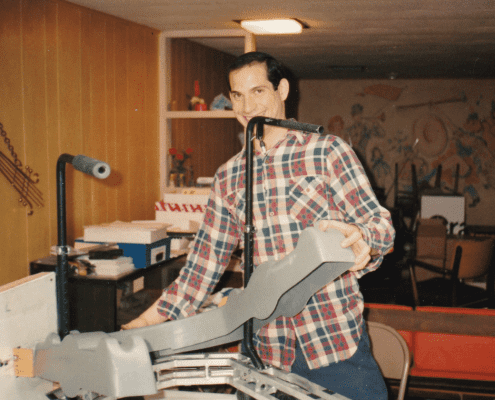
Journey from Prototype to Production: Part 1
These are pictures of the first U-Step, circa 1992. This was…

When You Can’t Be With Your Loved Ones This Holiday Season
December 2020. A challenging time to be celebrating the holidays.…
A Time to Give Thanks
"Life gets better the more you decide to take it easy on yourself."
-…

More Answers Than Questions for Individuals with MS: Should I "Give In" and Use an Assistive Device?
This may seem like a tough question – but it has a surprisingly…

Harnessing the Power of Telehealth for Physical Therapy
A couple of weeks ago, UStep participated in an important webinar…

Ice Cream Sundaes - Supporting Individuals with PSP
Eating ice cream is such good fun and is the special ingredient…

Our Foundation Partners: Easing the Burden of Parkinson’s Disease
We are living in challenging times.
This may be the understatement…

Taking Care in the Days of Telehealth
“Movement is a medicine for creating change in a person's physical,…
How Corona Took In-Step by Storm
“No company, small or large, can win over the long run without…

Finding the Right Community
The health and safety of our clients is of utmost importance…
Helping Individuals Cope with Ataxia
“Over the weekend I participated in my first 5K. I walked…and…

“Am I your only customer?”
“Am I your only customer?” she innocently asked. Katie* was…

Grandpa doesn't need another sweater...
It’s holiday time, and while it’s great fun shopping for…

How to Get Your U-Step Covered by Medicare
Many years ago when I first engineered the U-Step, I was a young…

Stop Freezing, Start Walking
U-Step has officially launched its newest product: LaserCue.…

Q&A for Your First Mobility Device
When it’s time for someone to begin using a mobility device,…
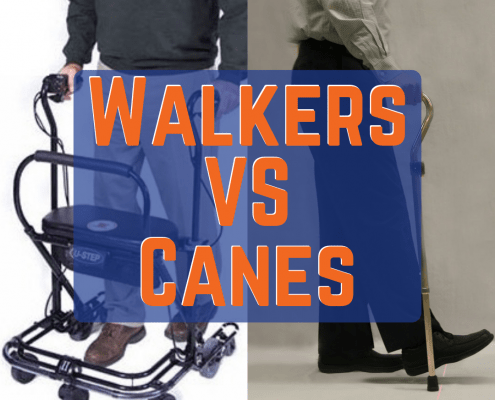
Choosing a Mobility Device: Canes vs. Walkers
When buying a mobility device for the first time, there is a…

A Company with Heart
I like to think of U-Step as a company driven by the heart. Our…

Parkinson’s and Depression
Depression is often the number one factor negatively impacting…

What You Need to Know About Parkinson's
It’s Parkinson’s Awareness Month! While not all, but many…
A Walker as Unique as You Are
Parkinson’s Awareness month is coming up in just a few days…

Avoid the Risks, Avoid the Falls
In our January blog post, we discussed the scary prospects of…

Don't Wait Until It's Too Late: Falls are Dangerous
Falling is a major contributing factor to the deterioration and…

Holidays, Family Time and those “Hard Conversations”
The holiday season is a time for great joy, family gatherings,…

Advancements in Parkinson’s Early Detection
Over the past several months, a surprising number of new innovations…

The Power of Physical Therapy
In honor of physical therapy month, we at Ustep want to celebrate…

What a Difference One Little Red Line Makes: Explaining Parkinson’s Freezing and How Cues Help
2 Comments
/
There are many things in life we take for granted until there…

The Gift of Walking
If you are a customer of ours, it is likely that you have been…

Finding the Right Kind of Support
Every new day brings opportunities for people to experience the…

My Spouse Has Been Diagnosed with Parkinson’s Disease - What Now?
The past few weeks of your life have felt like a whirlwind. You…

The U-Step Story: How the Company Began
I grew up with a mother who had trouble walking. She was born…