Posts

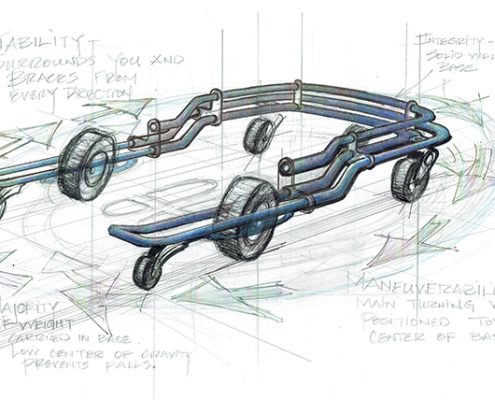
Journey from Prototype to Production: Part 1
These are pictures of the first U-Step, circa 1992. This was…

Ice Cream Sundaes - Supporting Individuals with PSP
Eating ice cream is such good fun and is the special ingredient…

Our Foundation Partners: Easing the Burden of Parkinson’s Disease
We are living in challenging times.
This may be the understatement…

Grandpa doesn't need another sweater...
It’s holiday time, and while it’s great fun shopping for…

Stop Freezing, Start Walking
U-Step has officially launched its newest product: LaserCue.…

A Company with Heart
I like to think of U-Step as a company driven by the heart. Our…

Parkinson’s and Depression
Depression is often the number one factor negatively impacting…

What You Need to Know About Parkinson's
It’s Parkinson’s Awareness Month! While not all, but many…
A Walker as Unique as You Are
Parkinson’s Awareness month is coming up in just a few days…

Advancements in Parkinson’s Early Detection
Over the past several months, a surprising number of new innovations…

What a Difference One Little Red Line Makes: Explaining Parkinson’s Freezing and How Cues Help
2 Comments
/
There are many things in life we take for granted until there…